A National Step Forward for Brain Health
A National Step Forward for Brain Health

Food for the Brain awarded an Innovate UK grant to advance early dementia detection and prevention
We are delighted to announce that Food for the Brain Foundation has been awarded a prestigious grant from Innovate UK, part of UK Research and Innovation (UKRI) – national recognition of our pioneering work in dementia prevention and early detection.
Importantly, this funding marks a milestone for us as a UK-based research charity. It also represents a significant step forward for our global community of citizen scientists, clinicians, and individuals dedicated to preventing Alzheimer’s, dementia, and cognitive decline.
For us, this is not just a charity and research achievement – it’s a sign that the world is waking up to prevention.
Why this matters?
Right now, someone in the UK develops dementia every three minutes. Across the globe, it’s every three seconds. And despite this, dementia cost the world over US$1.3 trillion in 2019, yet countless cases remain undiagnosed.
For nearly two decades, we have led the charge in prevention. So far, over 400,000 people worldwide have taken our Cognitive Function Test (CFT) – a free, validated online tool that helps you understand your brain health, assess your risks, and take action to improve.
This grant from Innovate UK, part of the UK’s national innovation agency, provides crucial funding to further validate and expand our tools for early dementia detection and – ultimately – prevention.
It forms part of the Blood Biomarker Challenge, a UK-wide research initiative, which aims to integrate blood-based biomarker testing into NHS diagnostic pathways.
Our Cognitive Function Test (CFT) has been selected to assess cognitive performance in the READ-OUT trial – part of this Innovate UK-funded programme, supported by the Department of Health and Social Care, the NIHR, and Alzheimer’s Research UK.
It will allow us to:
- Integrate our Cognitive Function Test into NHS-linked research, workflows, and clinical studies, thereby bridging science and healthcare delivery.
- Further expand access to our evidence-based prevention tools – making them mobile-friendly, multilingual, and culturally inclusive for global use.
About Innovate UK
Innovate UK is the UK government’s innovation agency, supporting organisations that deliver real-world impact across science, technology, and health. Each year, it invests over £1 billion in ideas that can transform industries, economies, and lives – from sustainable energy and biotech to healthcare innovation.
Receiving an Innovate UK grant means your project has been rigorously evaluated for its scientific quality, innovation, feasibility, and potential global impact.

“This project marks a step-change in how we approach dementia,” said Emma George, CEO of the Food for the Brain Foundation. “With Innovate UK’s support, we can validate the Cognitive Function Test within the NHS and move closer to a future where true prevention, by protecting brain health, is routine and accessible to all.”
Emma George, CEO, Food for the Brain Foundation
What this means for global brain health and dementia detection?
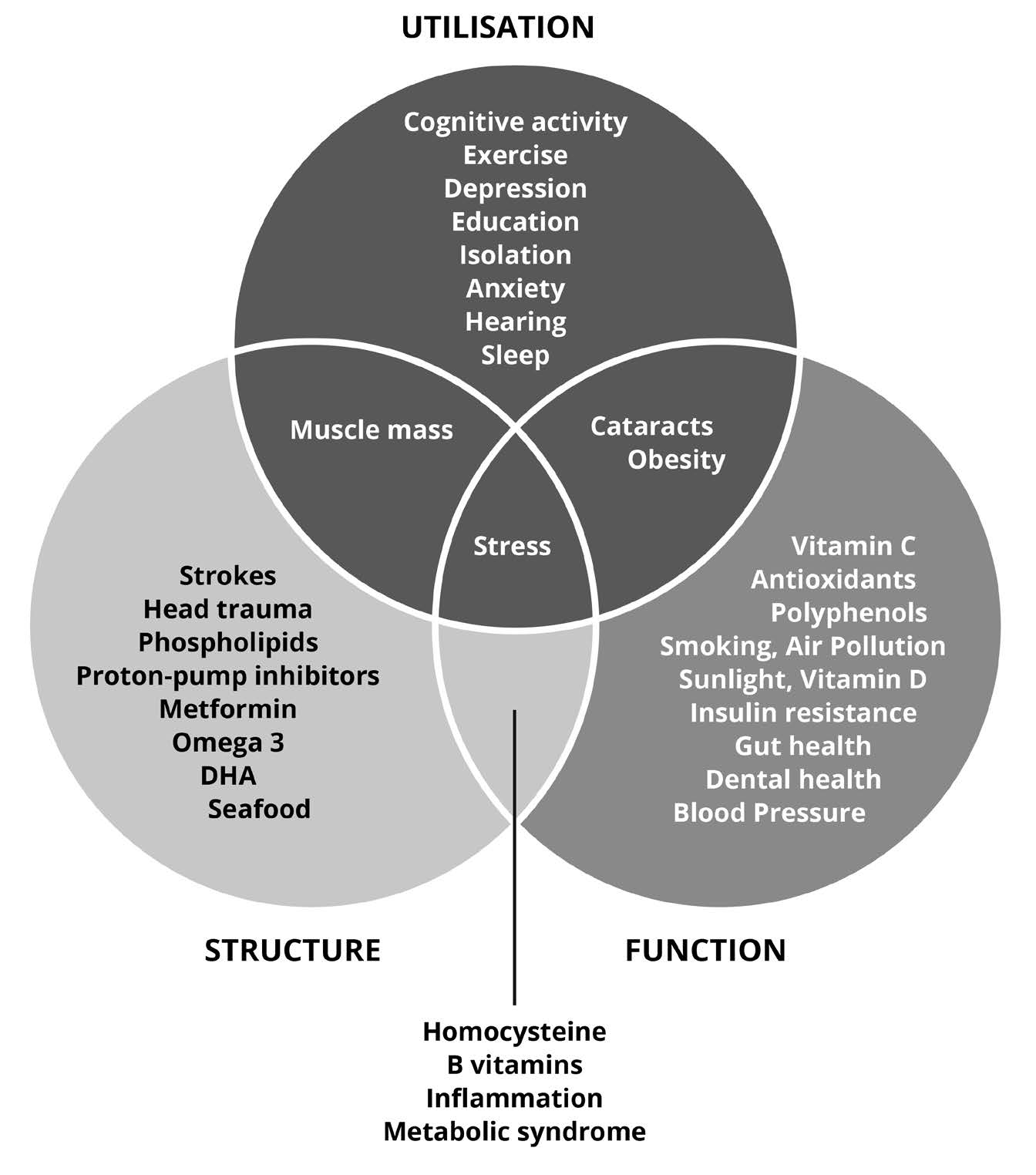
Our Cognitive Function Test (CFT) is the only freely available online tool that measures cognitive performance. It also provides a personalised Dementia Risk Index, based on eight key lifestyle and biological factors.
With this grant, we can now take the next step – integrating this digital test with blood test data from our DRIfT (Dementia Risk Index Functional Test).
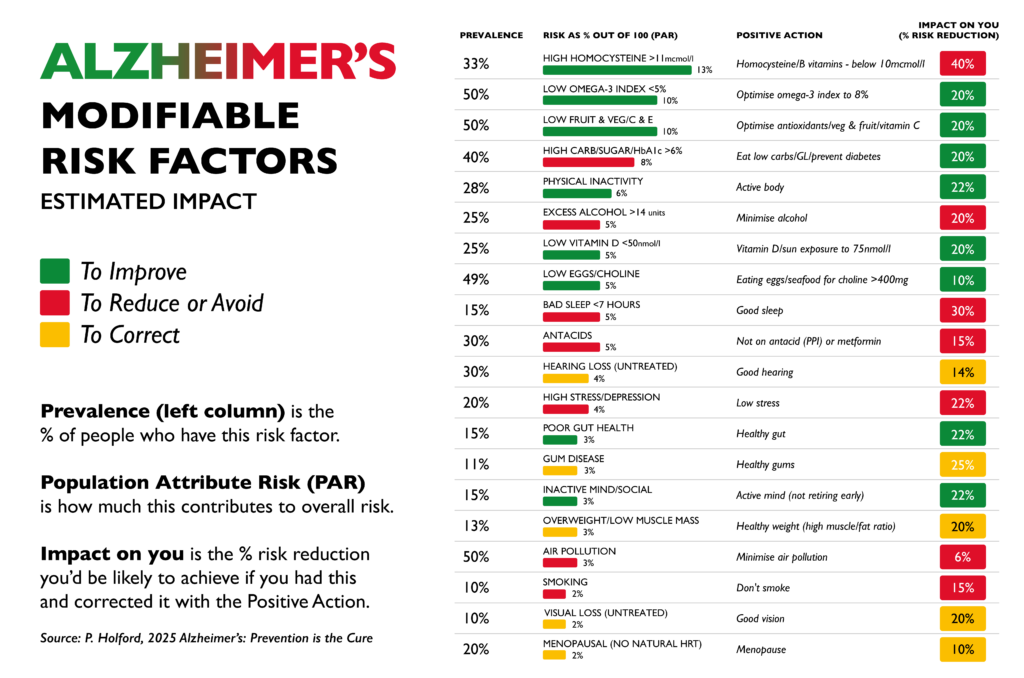
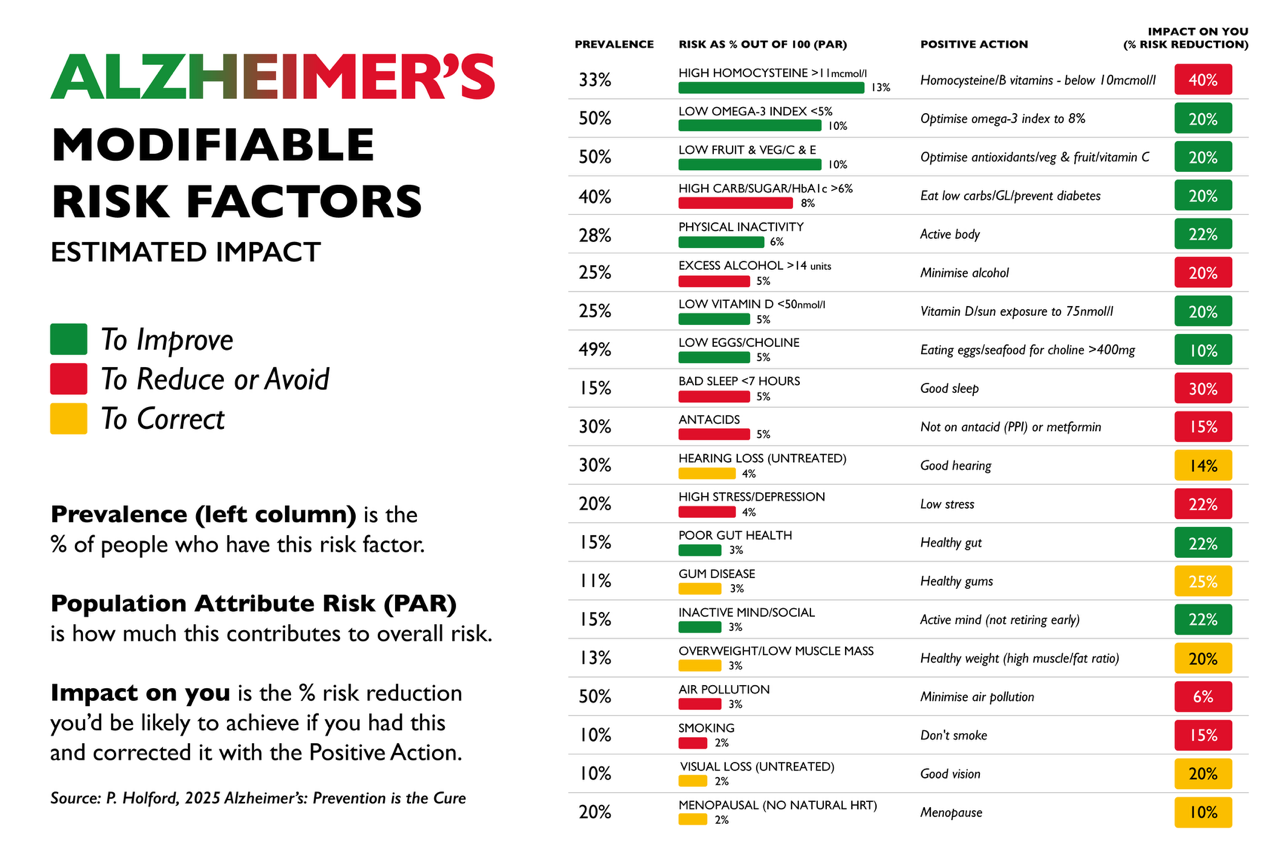
The DRIfT test measures five critical nutritional biomarkers proven to influence cognitive ageing:
- Omega-3 Index – vital brain fats that support memory and neuronal health
- Vitamin D – essential for mood, immunity, and brain protection
- Homocysteine – a marker of B-vitamin status; high levels increase the risk of brain shrinkage
- HbA1c – a measure of long-term blood sugar control linked to brain energy supply
- Glutathione Index – the body’s master antioxidant defence
Combining these markers with our multilingual, free Cognitive Function Test means that more and more people can detect early warning signs of cognitive decline. This can happen decades before diagnosis. This empowers them to take action early – and prevent it. Together, these innovations represent the future of dementia detection and prevention.
Why prevention and early dementia detection must come first?
Despite billions spent on drug development, no Alzheimer’s medication to date has shown meaningful improvement in cognitive outcomes. In fact, many come with serious side effects, including brain swelling and bleeding. (Read more Alzheimer’s drugs here and here.)
That’s why our focus, and now Innovate UK’s, is on early dementia detection.
Identifying risk early, addressing nutritional and metabolic imbalances, and protecting the brain before damage occurs.

“For nearly two decades we’ve been proving that Alzheimer’s is preventable. This grant allows us to bring that proof into mainstream healthcare and make prevention available to all.”
Patrick Holford, Founder, Food for the Brain Foundation
Take part – protect your brain, advance the science, stay sharp for life
Ultimately, this work only matters if people like you take part.
By joining our global citizen-science movement, you’ll help us refine and accelerate the world’s first large-scale dementia prevention database.
Step 1: Take the free Cognitive Function Test
A quick, 20-minute online test that shows you how well your brain is performing and what to do next.
Step 2: Complete the DRIFT biomarker test
A simple at-home finger-prick blood test that measures your omega-3, vitamin D, B-vitamin, blood sugar, and antioxidant status.
Step 3: Become a FRIEND of Food for the Brain
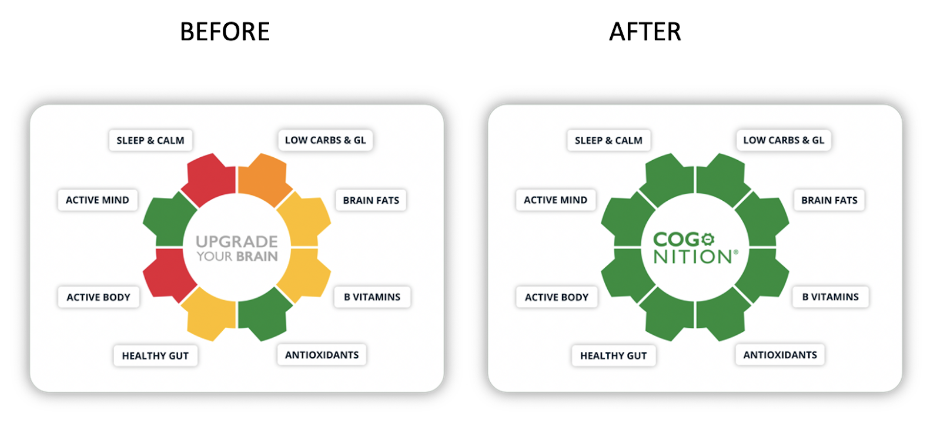
For just £50 a year or £5 a month, you can support our research and charitable work. You’ll also gain access to ![]() – your personalised brain upgrade programme. Additionally, enjoy monthly group coaching sessions and live webinars.
– your personalised brain upgrade programme. Additionally, enjoy monthly group coaching sessions and live webinars.
Looking ahead: the future of dementia detection and prevention
With the support of Innovate UK, the NHS, and thousands of citizen scientists and Friends, we’re building a future where Alzheimer’s is preventable, not inevitable.
Ultimately, this grant strengthens our ability to deliver credible, evidence-based tools that empower everyone to take charge of their cognitive health – starting today.
Take the test. Join the study. Be part of prevention.
👉 foodforthebrain.org/tests | foodforthebrain.org/driftstudy
Food for the Brain is a not-for-profit educational and research charity that offers a free Cognitive Function Test and assesses your Dementia Risk Index to be able to advise you on how to dementia-proof your diet and lifestyle.
By completing the Cognitive Function Test you are joining our grassroots research initiative to find out what really works for preventing cognitive decline. We share our ongoing research results with you to help you make brain-friendly choices.
Please support our research by becoming a Friend of Food for the Brain.
Reference: