Psychiatric Drugs Are The Third Leading Cause Of Death
By Patrick Holford
—
Unspoken Risks of Psychiatric & Dementia Drugs
A similar situation is emerging with the new anti-amyloid antibody treatments being proposed for dementia sufferers. Reported deaths are often downplayed or not fully disclosed.. In trials of the two drugs Lecanemab and Donanemab, eight deaths were reported. Eight deaths were reported during the trials, which involved 1,785 participants – a rate of one in every 219 – though not all were officially attributed to the drug. That’s quite a risk. But it is also the nature of these deaths, caused by brain bleeding and swelling, that is even more concerning.
Investigative journalist Charles Piller, in his book ‘Doctored’, interviewed the pathologist for the first Lecanemab death who said it was like “her brain exploded”. Another Lecanemab associated death was a 65 year-old woman, who had a blood clot induced stroke and was given a common, often lifesaving intervention (tPA) which went badly wrong. “As soon as they put it in her, it was like her body was on fire,” the woman’s husband told me, he said. “She was screaming, and it took, like, eight people to hold her down. It was horrific. Everybody’s running in and (asking) ‘What the hell is going on?’” His wife was sedated and recovered to intensive care, he said. Soon the woman suffered seizures and was placed on a ventilator. After a few days the family approved disconnecting the device and she died. In his book Piller also reports another case in which a participant ‘died after hideous brain swelling and bleeding, and violent seizures.’
The UK has licensed the use of Lecanemab. The EU has not. The UK has licensed Donanemab, but NICE hasn’t approved it for NHS use.
Safer, Evidence-Based Alternatives
We invited Dr Peter Gøtzsche – co-founder of the Cochrane Collaboration, originally established to evaluate health treatments without bias – to speak about the risks of psychiatric drugs and their link to mortality. When the Cochrane Collaboration became corrupted, which he later criticised for being influenced by commercial interests, he founded the Institute for Scientific Freedom.
“Overtreatment with drugs kills many people, and the death rate is increasing. It is therefore strange that we have allowed this long-lasting drug pandemic to continue, and even more so because most of the drug deaths are easily preventable.” he says.
“In 2013, I estimated that our prescription drugs are the third leading cause of death after heart disease and cancer,(1) and in 2015, that psychiatric drugs alone are also the third leading cause of death”.(2)”
How many people are killed by psychiatric drugs?
If we want to estimate the death toll of psychiatric drugs, the most reliable source of data comes from placebo-controlled randomised trials. However, we need to consider their limitations.
First, these trials typically last just a few weeks, despite the fact that most patients take psychiatric medications for many years.(3, 4)
Second, polypharmacy – the use of multiple medications – is common in psychiatry, and this significantly increases the risk of mortality.. As an example, the Danish Health Authority has warned that adding a benzodiazepine to a neuroleptic increases mortality by 50-65% (5).
Third, up to half of all deaths go unreported in published clinical trial data.(6) For dementia, published data shows that for every 100 people treated with a newer neuroleptic for ten weeks, one patient dies as a result. (7) This represents a high mortality rate for a pharmaceutical intervention, but FDA data on the same trials show it is double this number, equivalent to two deaths per 100 people over ten weeks. (8) And if we extend the observation period, the death toll becomes even higher. A Finnish study of 70,718 community-dwellers newly diagnosed with Alzheimer’s disease reported that neuroleptics kill 4-5 people per 100 annually, compared to patients who were not treated.(9)
Fourth, the design of psychiatric drug trials is biased. In almost all cases, patients were already in treatment with psychiatric medication before they entered the trial, (1, 2), and some of those randomised to placebo will therefore experience withdrawal effects that will increase their risk of dying, due to withdrawal symptoms such as akathisia. Placebo-controlled trials in schizophrenia cannot be reliably used to assess the effect of neuroleptics on mortality because of the drug withdrawal design. The suicide rate in these unethical trials was 2-5 times higher than the norm. (10,11) Among those enrolled in trials of risperidone, olanzapine, quetiapine, and sertindole, one in every 145 patients died. However, none of these deaths were mentioned in the published scientific literature, and the FDA did not require their inclusion in trial reporting.
Fifth, events occurring after the trial period are often ignored. In Pfizer’s trials of sertraline in adults, the risk ratio for suicides and suicide attempts was 0.52 when follow-up lasted only 24 hours, but increased to 1.47 when follow-up was extended to 30 days — indicating a rise in suicidal events. (12) Furthermore, when researchers reanalysed the FDA trial data on depression drugs and included harms occurring during follow-up, they found that antidepressants were associated with twice the number of suicides in adults compared to placebo (13, 14)
Estimating the True Death Toll of Mental-Health Medications
In 2013, I estimated that, in people aged 65 and above, neuroleptics, benzodiazepines or similar, and antidepressants kill 209,000 people annually in the United States.(2) I used relatively conservative estimates, however, and usage data from Denmark, which is far lower than those in USA. I have therefore updated the analysis based on US usage data, again focusing on older age groups.
For neuroleptics, I used the estimate of 2% mortality from the FDA data.(8)
For benzodiazepines and similar drugs, a matched cohort study showed that the drugs doubled the death rate, although the average age of the patients was only 55.(15) The excess death rate was about 1% per year. In another large, matched cohort study, the appendix to the study report shows that hypnotics quadrupled the death rate (hazard ratio 4.5). The study authors estimated that sleeping pills kill between 320,000 and 507,000 Americans every year. (16) A reasonable estimate of the annual death rate would therefore be 2%.
For SSRIs, a UK cohort study of 60,746 depressed patients older than 65 showed that they led to falls and a 3.6% annual mortality rate among those treated.(17) The study was well-designed, in that the patients were their own control in one of the analyses, which helps control for confounding variables. Nonetheless, the reported death rate is notably high.
Another cohort study, of 136,293 American postmenopausal women (age 50-79) participating in the Women’s Health Initiative study, found that depression drugs were associated with a 32% increase in all-cause mortality after adjustment for confounding factors, which corresponding to an estimated 0.5% annual mortality rate among women treated with SSRIs.(18). The authors noted that the mortality rate was likely underestimated. The authors warned that their results should be interpreted with great caution due to a high risk of exposure misclassification, which would make it more difficult to find an increase in mortality. Further, the patients were much younger than in the UK study, and the death rate increased markedly with age and was 1.4% for those aged 70-79. Finally, the exposed and unexposed women were different for many important risk factors for early death, whereas the people in the UK cohort were their own control.
For these reasons, I decided to use the average of the two estimates, a 2% annual death rate.
These are my results for USA for these three drug groups for people at least 65 years of age (58.2 million; usage is in outpatients only): (19, 20, 21, 22)
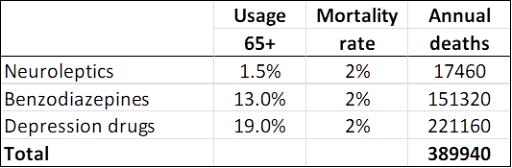
—
A limitation in these estimates is that you can only die once, and many people receive polypharmacy. It is not clear how we should adjust for this. In the UK cohort study of depressed patients, 9% also took neuroleptics, and 24% took hypnotics/anxiolytics. (17)
On the other hand, the data on death rates come from studies where many patients were also on several psychiatric drugs in the comparison group, so this is not likely to be a major limitation considering also that polypharmacy increases mortality beyond what the individual drugs cause.
Statistics from the Centers for Disease Control and Prevention list these four top causes of death: (23)
Heart disease: 695,547
Cancer: 605,213
COVID-19: 416,893
Accidents: 224,935
COVID-19 deaths are rapidly declining, and many of such deaths are not caused by the virus but merely occurred in people who tested positive for it because the WHO advised that all deaths in people who tested positive should be called COVID deaths.
Young people have a much smaller death risk than the elderly, as they rarely fall and break their hip, which is why I have focused on the elderly. I have tried to be conservative. My estimate misses many drug deaths in those younger than 65 years; it only included three classes of psychiatric drugs; and it did not include hospital deaths.
I therefore do not doubt that psychiatric drugs are the third leading cause of death after heart disease and cancer.
—
Learn more and begin your brain upgrade journey today:
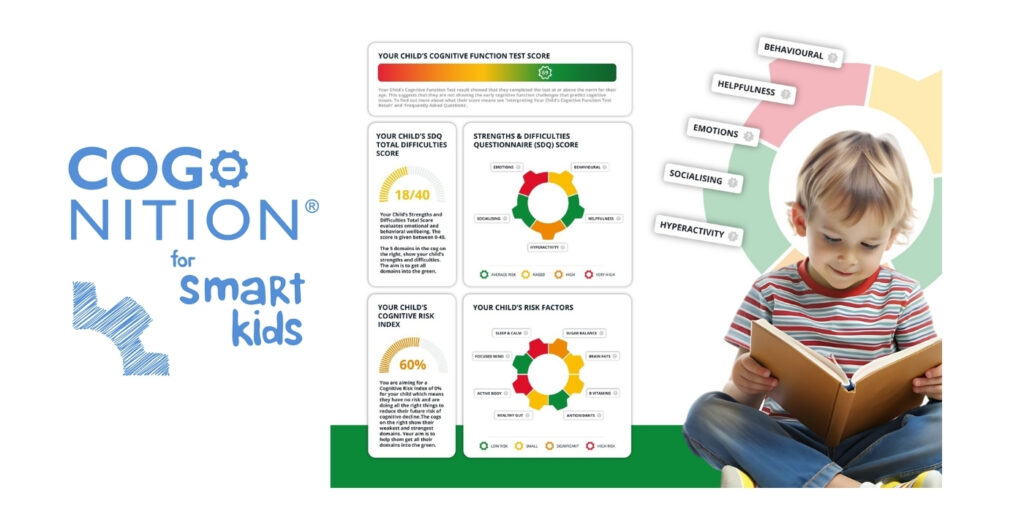
- Complete the free online brain assessment – the Cognitive Function Test – to get personalised feedback on your brain health
- Order the Upgrade Your Brain book here
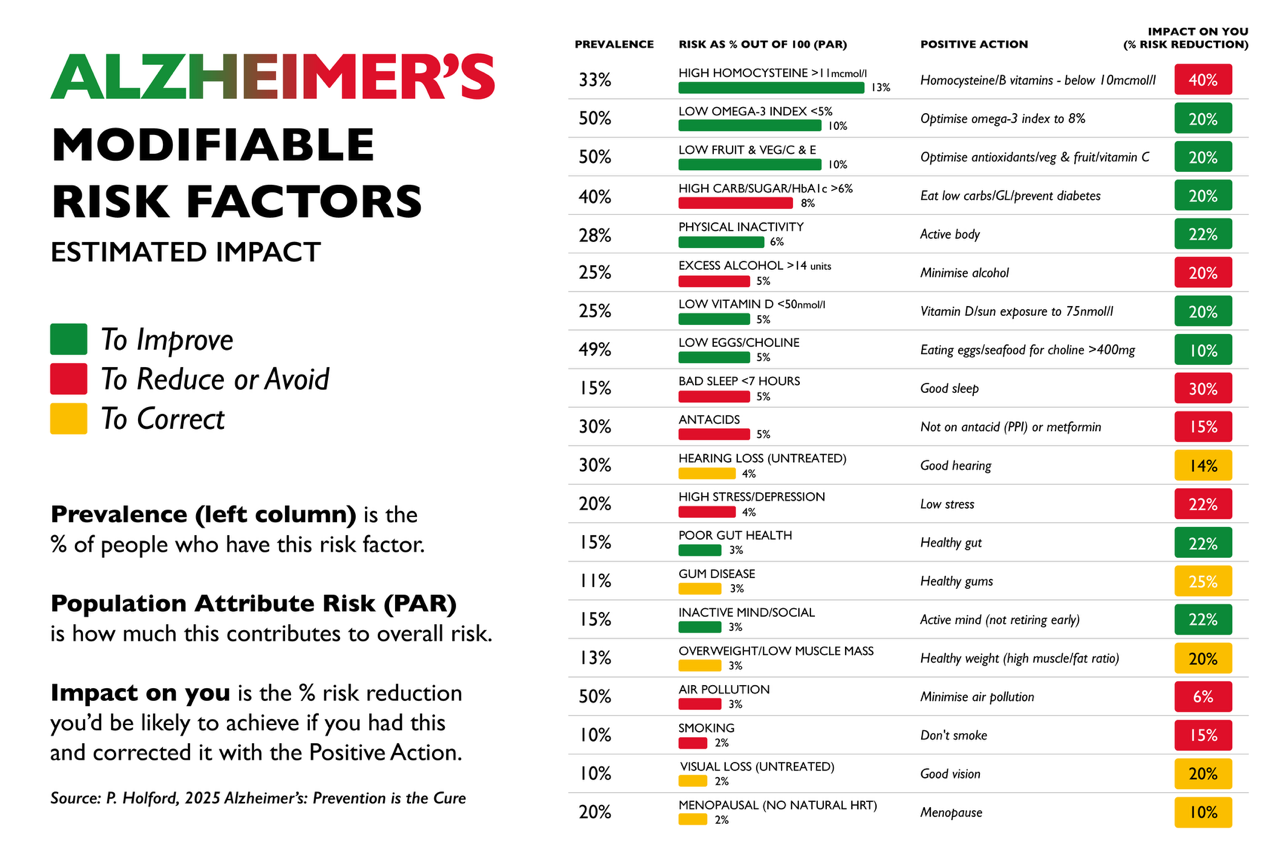
- Order Alzheimer’s: Prevention is the Cure book here
- Contribute to our research and order your accurate, at home, blood tests here.
- If you are looking for personalised one to one support, visit the Brain Bio Centre here.
—
2 Gøtzsche PC. Deadly psychiatry and organised denial. Copenhagen: People’s Press; 2015.. US News 2016; Sept 27.
2. Gøtzsche PC. Mental health survival kit and withdrawal from psychiatric drugs. Ann Arbor: L H Press; 2022.
3 Gøtzsche PC. Long-term use of antipsychotics and antidepressants is not evidence-based. Int J Risk Saf Med 2020;31:37-42.
4 Gøtzsche PC. Long-term use of benzodiazepines, stimulants and lithium is not evidence-based. Clin Neuropsychiatry 2020;17:281-3.
5 Forbruget af antipsykotika blandt 18-64 årige patienter, med skizofreni, mani eller bipolar affektiv sindslidelse. København: Sundhedsstyrelsen; 2006.
6 Hughes S, Cohen D, Jaggi R. Differences in reporting serious adverse events in industry sponsored clinical trial registries and journal articles on antidepressant and antipsychotic drugs: a cross-sectional study. BMJ Open 2014;4:e005535.
7 Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA 2005;294:1934–43.
8 FDA package insert for Risperdal (risperidone). Accessed 30 May 2022.
9 Koponen M, Taipale H, Lavikainen P, et al. Risk of mortality associated with antipsychotic monotherapy and polypharmacy among community-dwelling persons with Alzheimer’s disease. J Alzheimers Dis 2017;56:107-18.
10 Whitaker R. Lure of riches fuels testing. Boston Globe 1998;Nov 17.
11 Whitaker R. Mad in America: bad science, bad medicine, and the enduring mistreatment of the mentally ill. Cambridge: Perseus Books Group; 2002:page 269.
12 Vanderburg DG, Batzar E, Fogel I, et al. A pooled analysis of suicidality in double-blind, placebo-controlled studies of sertraline in adults. J Clin Psychiatry 2009;70:674-83.
13 Hengartner MP, Plöderl M. Newer-generation antidepressants and suicide risk in randomized controlled trials: a re-analysis of the FDA database. Psychother Psychosom 2019;88:247-8.
14 Hengartner MP, Plöderl M. Reply to the Letter to the Editor: “Newer-Generation Antidepressants and Suicide Risk: Thoughts on Hengartner and Plöderl’s ReAnalysis.” Psychother Psychosom 2019;88:373-4.
15 Weich S, Pearce HL, Croft P, et al. Effect of anxiolytic and hypnotic drug prescriptions on mortality hazards: retrospective cohort study. BMJ 2014;348:g1996.
16 Kripke DF, Langer RD, Kline LE. Hypnotics’ association with mortality or cancer: a matched cohort study. BMJ Open 2012;2:e000850.
17 Coupland C, Dhiman P, Morriss R, et al. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 2011;343:d4551.
18 Smoller JW, Allison M, Cochrane BB, et al. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women’s Health Initiative study. Arch Intern Med 2009;169:2128-39.
19 O’Neill A. Age distribution in the United States from 2012 to 2022. Statista 2024;Jan 25.
20 Olfson M, King M, Schoenbaum M. Antipsychotic treatment of adults in the United States. Psychiatrist.com 2015;Oct 21.
21 Maust DT, Lin LA, Blow FC. Benzodiazepine use and misuse among adults in the United States. Psychiatr Serv 2019;70:97-106.
22 Brody DJ, Gu Q. Antidepressant use among adults: United States, 2015-2018. CDC 2020;Sept.