Four Quick Wins to Reduce Your Risk of Alzheimer’s

—
What can you do, practically and quickly, to reduce your risk of developing Alzheimer’s?
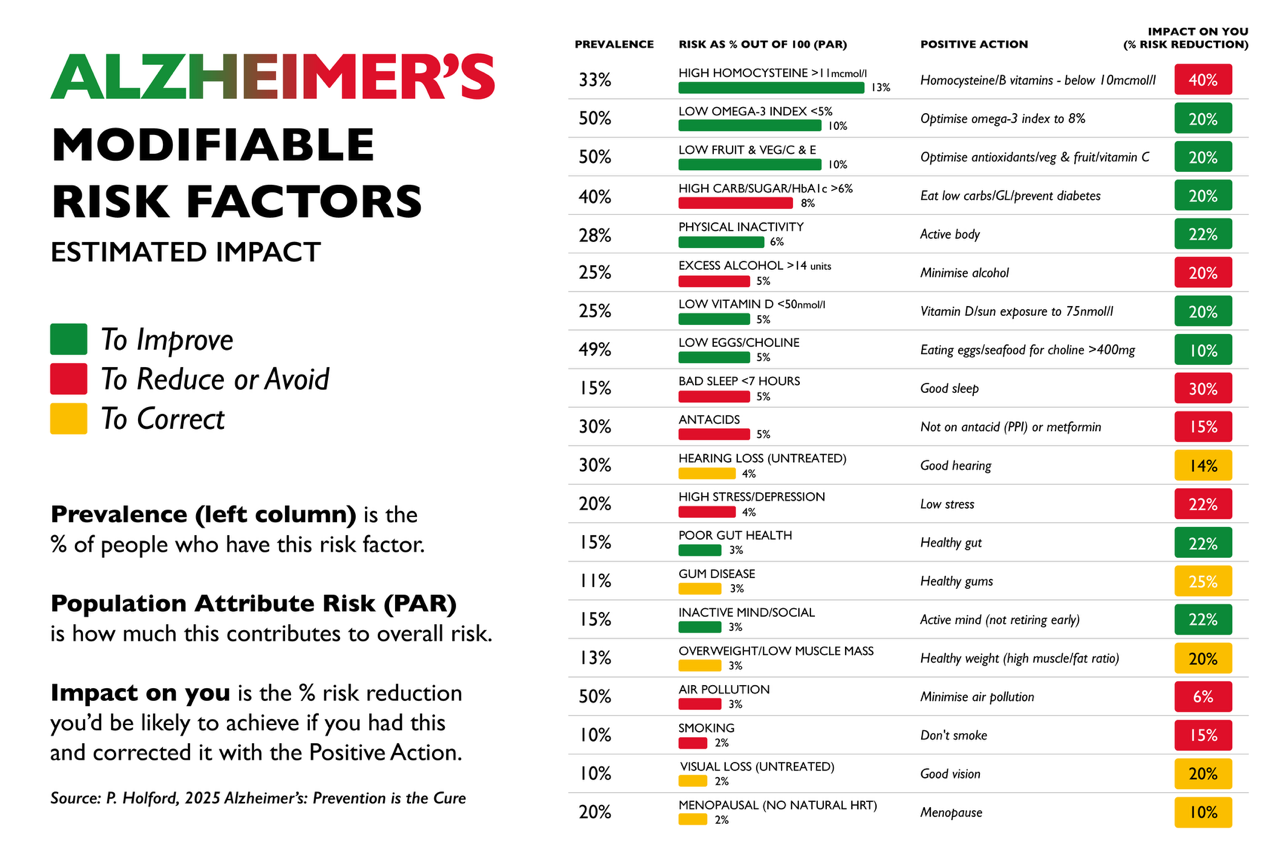
The International Alzheimer’s Prevention Expert Group, including our founder Patrick Holford, has identified four key areas that could cut your future risk by over 80% – down to less than a quarter – if addressed early.
The four “quick wins”? Increase your vitamin D, omega-3, and B vitamins, and reduce your intake of sugar and refined carbs.
1. Vitamin D: The Sunshine Factor
Vitamin D is primarily made in your skin through sun exposure, particularly at midday in the summer. However, in the winter – especially in the UK and other northern countries – you cannot make enough, so supplementation is essential. A Dutch study found that people with low levels of vitamin D, omega-3s, and B vitamins were over four times more likely to develop dementia¹. Those who supplement with vitamin D have around a third less risk².
Even levels below 62.5 nmol/L (25 ng/mL) increase risk. A French study found that low vitamin D levels tripled Alzheimer’s risk³. The darker your skin, the more sun exposure you need – which makes supplementation all the more vital for many.
2. Omega-3: Feed Your Brain with Fish
Fish is a true brain food – rich in omega-3s, vitamin D, and B12. Eating fish at least once a week reduces Alzheimer’s risk by a third⁴. A recent review confirmed that a daily serving cuts the risk of cognitive decline by 30%⁵.
Omega-3 fats (especially DHA) quite literally build brain cells. The UK Biobank study of over 250,000 people found that those with higher omega-3 levels had a 20% lower risk of dementia⁶. A US study also found that a higher omega-3 index correlated with more white matter in the brain and better cognitive function⁷.
Professor William Harris of the Fatty Acid Research Institute calls it “a safe, simple, cheap and effective tool to forestall Alzheimer’s.”
3. B Vitamins: The Brain Fixers
B6, B12, and folate don’t just support brain function – they’re essential for fixing omega-3s into your brain’s cell membranes. Without them, homocysteine – a toxic amino acid – builds up in your blood. High levels (above 11 μmol/L) are strongly linked to brain shrinkage and Alzheimer’s.
Half of people over 60 in the US have homocysteine levels above 11. The Dutch study found that risk rises even above 8 – a level many people exceed.
As Professor Joshua Miller from Rutgers University says, raised homocysteine is an early warning sign: “a canary in the coal mine.” The good news? It’s easily lowered with a B vitamin supplement – ideally one containing 500 mcg of B12, methylfolate, and B6.
More greens, beans, nuts, and lentils also help. A recent study showed that replacing just one serving of processed meat with nuts or beans (rich in folate) cut dementia risk by 19%⁸.
4. Sugar and Refined Carbs: Silent Brain Saboteurs
The more sugar a person eats – including refined white carbohydrate foods such as bread, pastries, pasta, and rice – the higher their risk of both diabetes and dementia. Fizzy drinks and ultra-processed foods, sweetened with high-fructose corn syrup, are particularly bad for the brain.
“The brain needs the most energy of any organ, so it has the most mitochondria to make it. Sugar damages mitochondria,” says Dr Robert Lustig from the University of California, San Francisco.
A study just published this month in Neurology involving 2 million people shows that those with sugar problems (metabolic syndrome) are 24% more likely to develop dementia early¹⁰.
Keeping blood glucose levels in the low–normal range is reflected by a low glycosylated haemoglobin (HbA1c), which is the blood test doctors use to diagnose diabetes. Having a lower HbA1c is associated with reduced risk for dementia in several studies⁹. A recent study of 374,021 older men with diabetes found that keeping HbA1c stable over three years cut the risk of dementia by a third¹¹.
Want to know what’s driving your brain risk?
Take our free 3-minute Alzheimer’s Prevention Check at alzheimersprevention.info – or, for the full picture, order the four-in-one home blood test to measure your omega-3 index, vitamin D, homocysteine and HbA1c: foodforthebrain.org/tests

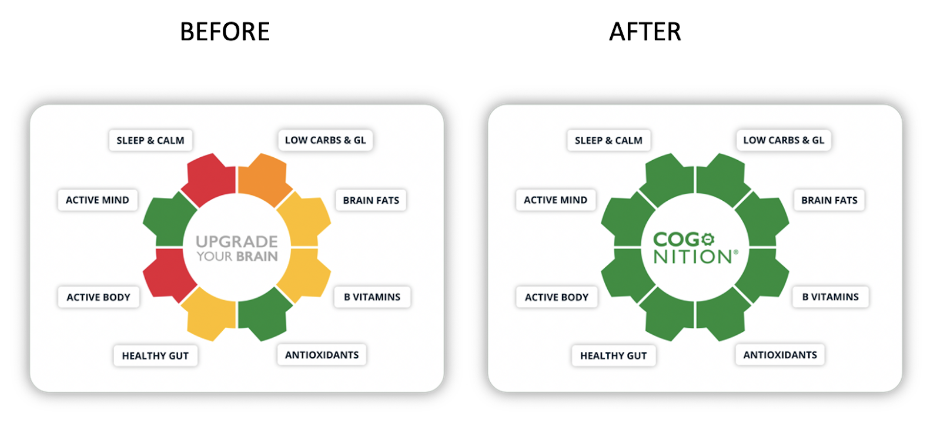
Food for the Brain is a not-for-profit educational and research charity that offers a free Cognitive Function Test and assesses your Dementia Risk Index to be able to advise you on how to dementia-proof your diet and lifestyle.
By completing the Cognitive Function Test you are joining our grassroots research initiative to find out what really works for preventing cognitive decline. We share our ongoing research results with you to help you make brain-friendly choices.
Please support our research by becoming a Friend of Food for the Brain.
References:
2 Ghahremani M, et al. Vitamin D supplementation and incident dementia: Effects of sex, APOE, and baseline cognitive status. Alzheimers Dement (Amst). 2023 Mar;15(1):e12404. doi: https://doi.org/10.1002/dad2.12404
3 Feart C, et al. Associations of lower vitamin D concentrations with cognitive decline and long-term risk of dementia and Alzheimer’s disease in older adults. Alzheimers Dement. 2017 Nov;13(11):1207-1216. doi: https://doi.org/10.1016/j.jalz.2017.03.003
4 Beydoun MA, et al. Epidemiologic studies of modifiable factors associated with cognition and dementia: systematic review and meta-analysis. BMC Public Health. 2014;14:643. doi: https://doi.org/10.1186/1471-2458-14-643
5 Godos J, et al. Fish consumption, cognitive impairment and dementia: an updated dose-response meta-analysis of observational studies. Aging Clin Exp Res. 2024;61:3731–3739. doi: https://doi.org/10.1007/s40520-024-02823-6
6 Sala-Vila A, et al. Plasma Omega-3 Fatty Acids and Risk for Incident Dementia in the UK Biobank Study: A Closer Look. Nutrients. 2023 Nov;15(23):4896.
7 Loong S, et al. Omega-3 Fatty Acids, Cognition, and Brain Volume in Older Adults. Brain Sci. 2023;13:1278. doi: https://doi.org/10.3390/brainsci13091278
8 Li Y, et al. Long-term intake of red meat in relation to dementia risk and cognitive function in US adults. Neurology.2025;104(3):e210286. doi: https://doi.org/10.1212/WNL.0000000000210286
9 Luchsinger JA, et al. Hyperinsulinemia and risk of Alzheimer disease. Neurology. 2004;63(7):1187–92. doi:https://doi.org/10.1212/01.WNL.0000140292.04932.04932.87; see also Abbatecola AM, et al. Insulin resistance and executive dysfunction in older persons. J Am Geriatr Soc.2004;52(10):1713–
8. https://doi.org/10.1111/j.1532-5415.2004.52466.x ;see also Xu WL, et al. Uncontrolled diabetes increases the risk of Alzheimer’s disease: a population-based cohort study. Diabetologia. 2009;52(6):1031–
9. doi: 10.1007/s00125-009-1323-x ;see also Hassing LB, et al. Type 2 diabetes mellitus contributes to cognitive decline in old age: a longitudinal population-based study. J Int Neuropsychol Soc. 2004;10(4):599–607. https://doi.org/10.1017/S1355617704104165
; see also Yaffe K, et al. Glycosylated hemoglobin level and development of mild cognitive impairment or dementia in older women. J Nutr Health Aging. 2006;10(4):293–5. https://pubmed.ncbi.nlm.nih.gov/16886099/ ; see also Roberts RO, et al. Diabetes and elevated hemoglobin A1c levels are associated with brain hypometabolism but not amyloid accumulation. J Nucl Med. 2014;55(5):759–64. https://jnm.snmjournals.org/content/55/5/759
10 Lee JY, Han K, Kim J, Lim JS, Cheon DY, Lee M. Association Between Metabolic Syndrome and Young-Onset Dementia: A Nationwide Population-Based Study. Neurology. 2025 May 27;104(10):e213599. doi: 10.1212/WNL.0000000000213599. Epub 2025 Apr 23. PMID: 40267374.11 Underwood PC, et al. HbA1c time in range and dementia. JAMA Netw Open. 2024;7(8):e2425354. doi: https://doi.org/10.1001/jamanetworkopen.2024.25354